By Dr. Fabio Zannoni, Gastroenterologist at Aventino Medical Group, Rome
Introduction
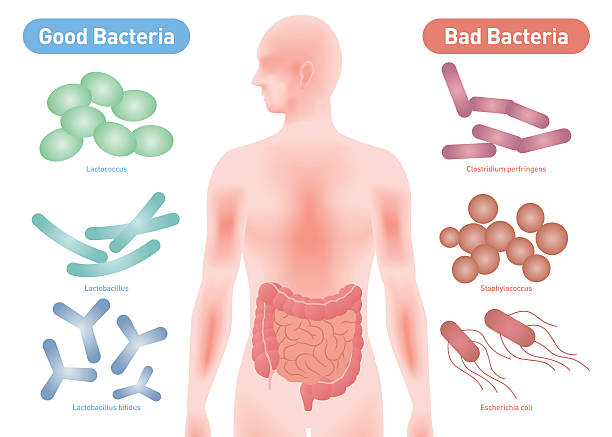
The intestinal microbioma is a complex ecosystem of billions of bacteria and other microorganisms that inhabit our gastrointestinal tract. This microscopic universe plays a crucial role in digestion, vitamin synthesis, and immune system balance. According to recent studies, a healthy microbioma promotes microbial biodiversity, reducing the risk of dysbiosis and preventing gastrointestinal disorders such as Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Diseases (IBD).
The key role of the microbioma in digestive health
A healthy gut is not just about good digestion—it is fundamental to overall health. The intestinal microbioma performs several essential functions:
- Digestion and nutrient absorption: It helps break down fiber and produces short-chain fatty acids, essential for energy and metabolism.
- Vitamin synthesis: Certain bacterial species produce vitamin K and B-group vitamins, crucial for many biological functions.
- Immune system regulation: About 70% of immune cells reside in the gut, where the microbioma plays a crucial role in modulating immune responses.
- Protection against pathogens: A balanced intestinal flora acts as a barrier against harmful bacteria and infectious agents.
- Impact on mental health: The gut-brain axis regulates cognitive and emotional aspects, influencing anxiety, depression, and stress levels.
Intestinal dysbiosis: symptoms and consequences
The intestinal microbioma serves as a barrier against pathogens that come into contact with our digestive system. It constantly stimulates the immune system, allowing it to tolerate beneficial microorganisms and recognize them as non-threatening.
Intestinal dysbiosis occurs when the balance between beneficial and pathogenic bacteria is disrupted. The most common causes include poor diet, stress, excessive antibiotic use, and a sedentary lifestyle.
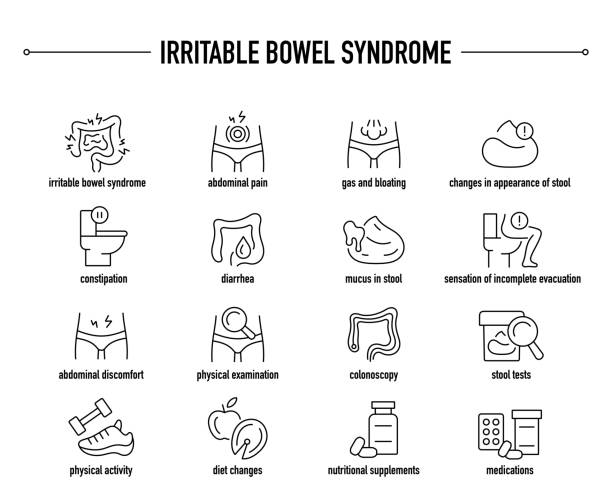
Some typical signs of microbioma imbalance include:
- Abdominal bloating and gas
- Chronic diarrhea or constipation
- Nutrient malabsorption and fatigue
- Recurring abdominal pain
- Mood disorders and anxiety
An altered microbioma has been linked to pathological conditions such as IBS, Crohn’s disease, ulcerative colitis, obesity, and type 2 diabetes.
Chronic inflammatory bowel diseases (IBD)—along with IBS, infectious enterocolitis, and food intolerances—are associated with microbioma alterations, increased intestinal permeability, and reduced microbial diversity. These imbalances stem from both genetic factors and microbiome changes.
Proton pump inhibitors (PPIs), one of the most commonly used medications for treating gastroesophageal reflux disease (GERD) and excessive stomach acid production, alter both the oral and intestinal microbioma.
How to improve and maintain a healthy intestinal microbioma
A proper diet and lifestyle are key to maintaining a balanced microbioma. Here are some effective strategies:
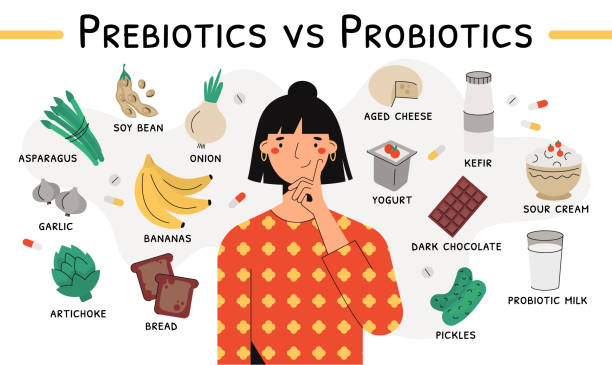
Follow a diet rich in prebiotic fibers
Some foods support the growth of beneficial bacteria, including:
- Prebiotics: Found in garlic, onions, leeks, asparagus, bananas, and legumes.
- Probiotics: Present in yogurt, kefir, miso, kimchi, and fermented sauerkraut.
- Polyphenols: Contained in green tea, cocoa, blueberries, and olive oil, promoting microbial diversity.
Avoid ultra-processed foods
Refined sugars, artificial sweeteners, and trans fats encourage the growth of harmful bacteria, disrupting gut balance.
Engage in regular physical activity
Moderate exercise helps promote microbioma biodiversity.
Limit unnecessary antibiotic use
Excessive antibiotic intake destroys beneficial gut flora. If antibiotic therapy is necessary, it is helpful to supplement the diet with probiotics afterward.
The microbioma and its impact beyond digestion
The gut microbioma does not just affect digestion—it also interacts with multiple medical fields, including:
- Gastroenterology: IBS, Crohn’s disease, ulcerative colitis.
- Immunology: Immune response, autoimmune diseases.
- Endocrinology: Obesity, diabetes, and metabolic syndrome.
- Neurology & Mental Health: Anxiety, depression, and chronic stress.
How can dysbiosis be diagnosed?
Diagnosis starts with carefully assessing the patient’s symptoms.
Tests include:
- Bloodwork and stool analysis, with additional specific tests for inflammation and celiac disease.
- Ultrasound of the intestinal loops and Magnetic Resonance Enterography (MRE), which provide a reliable intestinal evaluation but require an expert operator.
- Colonoscopy, which allows direct observation and biopsy of the colon lining and the removal of adenomatous polyps, recognized as precancerous lesions.
Frequently asked questions (FAQ) about the gut microbioma
What are the signs of a balanced microbioma?
A healthy gut is reflected in regular digestion, absence of bloating, and good sleep quality.
Which foods harm the microbioma?
Processed foods, refined sugars, and artificial sweeteners can disrupt the gut flora.
Are probiotics really effective?
Yes, but they must be taken in specific strains suited to individual needs. It is always advisable to consult a specialist.
How long does it take to rebalance the microbioma?
Improvements can be seen within 2-4 weeks of lifestyle changes.

Conclusion
Maintaining a healthy gut microbioma is essential for digestive and overall well-being. By following a balanced diet, engaging in regular physical activity, and managing stress effectively, we can enhance gut health and prevent numerous diseases.
At Aventino Medical Group in Rome, our team of gastroenterologists offers in-clinic, remote, and at-home specialist consultations to provide personalized and comprehensive care.For more information or to book an appointment with Dr. Fabio Zannoni, visit his page here.
